Diagnosis of Pancreatic Cancer

CT
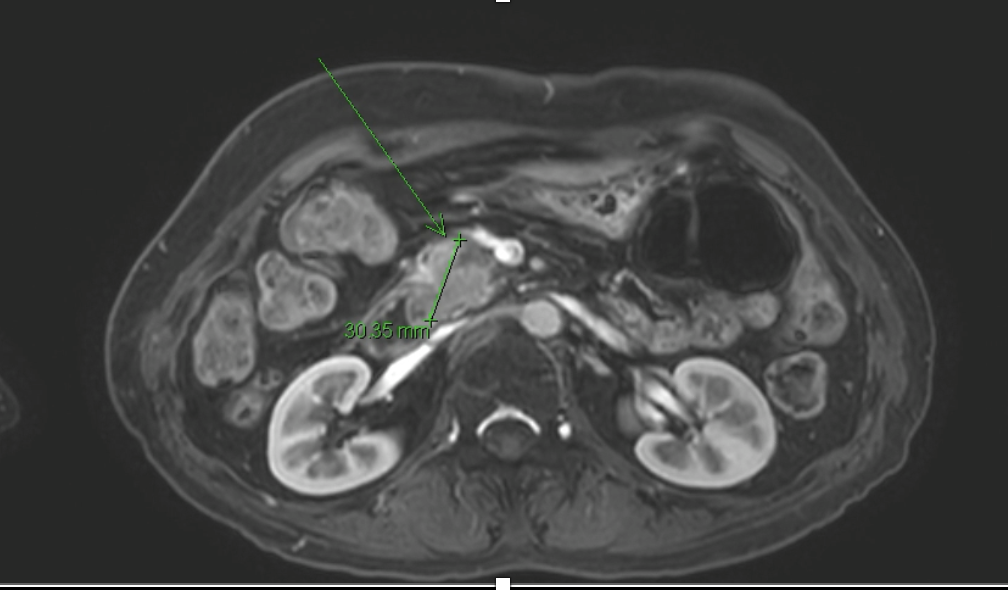
MRI

EUS-guided biopsy
1. Multiphase CT and MRI
- These are standard first-line imaging techniques that provide high-resolution visualization of pancreatic masses, local invasion, and metastatic spread.
- Multiphase CT (pancreatic protocol) remains the backbone for tumor staging and surgical planning.
- MRI, particularly with MRCP and diffusion-weighted imaging, offers superior soft tissue contrast and is especially helpful in detecting is attenuating tumors. It also enables non-invasive visualization of the pancreatic duct and bile duct, making it highly valuable in evaluating ductal obstruction. Furthermore, MRI is preferred in patients with renal impairment or iodine contrast allergy and provides multiparametric data that can aid in tumor characterization and staging.
2. Endoscopic Ultrasound (EUS)
- Endoscopic ultrasound (EUS) provides high-resolution, real-time imaging of the pancreas and surrounding structures. It is particularly valuable for detecting small or deeply located pancreatic lesions and guiding further diagnostic procedures.
3. Histological Tissue Biopsy (EUS-FNA/B, ERCP sampling)
- Definitive diagnosis remains reliant on pathology examination of tissue samples. EUS guided fine-needle aspiration and biopsies or ERCP-based ductal brushings and biopsies are commonly used.
4. Blood samples
- Traditional tumor markers like CA?19-9 and CEA are included in the diagnostic work-up but have limitations in sensitivity and specificity.
- Liquid biopsy techniques like circulating tumor DNA (ctDNA) and exosome analysis can detect molecular fingerprints of tumors with minimal invasiveness, and are being evaluated for high-risk screening.
Stages of Pancreatic Cancer
Pancreatic Cancer Staging (AJCC 8th Edition)
Pancreatic cancer staging helps determine the extent of disease and guides treatment planning. The American Joint Committee on Cancer (AJCC) 8th edition defines stages based on tumor size (T), lymph node involvement (N), and distant metastasis (M).
Stage 0 – Carcinoma in Situ (Tis; N0; M0)
Abnormal (pre-cancerous) cells are found in the lining of the pancreatic ducts. These cells have not invaded deeper tissues or spread. This stage is also called carcinoma in situ and may develop into invasive cancer over time.
Stage I – Localized Disease (T1–T2; N0; M0)
Cancer is confined to the pancreas and has not spread to lymph nodes or distant sites.
- Stage IA: The tumor is 2 cm or smaller (T1).
- Stage IB: The tumor is larger than 2 cm but not more than 4 cm (T2).
Stage II – Locally Advanced without Distant Spread
The tumor may be larger and/or may have spread to nearby lymph nodes, but not to distant organs.
- Stage IIA: Tumor is >4 cm but has not spread to lymph nodes (T3; N0; M0).
- Stage IIB: Tumor of any size (T1–T3) has spread to 1–3 regional lymph nodes (N1), but not to distant sites.
Stage III – Locally Advanced with Extensive Nodal or Vascular Involvement
The cancer involves major arteries near the pancreas (e.g., celiac axis or superior mesenteric artery), or has spread to 4 or more regional lymph nodes.
- Includes T4 tumors (involving major vessels) or any tumor with N2 nodal status (≥4 regional lymph nodes), but no distant metastasis (M0).
Stage IV – Metastatic Disease (Any T; Any N; M1)
The cancer has spread to distant sites such as the liver, lungs, or peritoneal cavity. Tumor size and lymph node status may vary, but the presence of distant metastasis defines this stage.